Neurology Residency Curriculum and Didactics

Morning Report with Program Director
Didactics
Orientation: One week of orientation lectures from senior residents, faculty, and ancillary staff. We cover a range of essential topics, from basics of neurology to the latest advancements in diagnosis and treatment.
Weekly lectures:
- Morning Reports
- Basic Sciences/Neuroanatomy
- Neurophysiology Lectures - alternate between epilepsy and neuromuscular topics
- Grand Rounds - includes various topics from our Neurology Faculty alternating between General Neurology, Neurovascular, Neurosurgery, and Tumor Board
Monthly lectures:
- Headache lecture series
- Case Based Learning with subspecialty faculty
- Wildcard Guest Lectures - covering topics including radiology, infectious disease, rheumatology, sleep disorders, otology, oncology, toxicology, pathology, nuclear neurology, etc.
- Research Meetings
Quarterly lectures:
- M&M
- Journal Clubs
RITE Prep: weekly starting in November held by the senior residents.

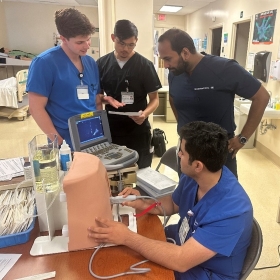

Botox Simulation on Mannequin Ultrasound Guided Spinal Tap
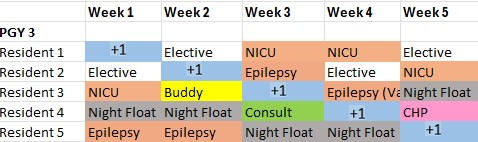
Example schedule
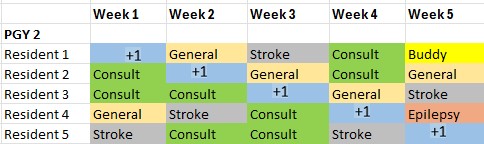
PGY 2
- General Neurology Service: 2-3 months
- Stroke Service: 10 weeks
- Consult Service: 8 weeks
- Night Float: 6 weeks
- Buddy: 2 weeks
- Epilepsy: 4 weeks
- Elective & Outpatient Clinic: 10 weeks
PGY 3
- General Neurology Service: 4 weeks
- Stroke Service: 4 weeks
- Consult Service: 2 weeks
- Night Float: 4 weeks
- NICU: 4 weeks
- Buddy: 4 weeks
- Epilepsy: 2 weeks
- Elective & Outpatient Clinic: 18 weeks
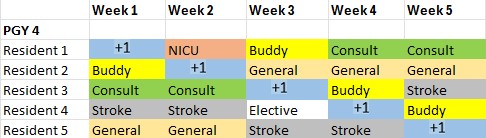
PGY 4
- General Neurology Service: 4 weeks
- Stroke Service: 4 weeks
- Consult Service: 3 weeks
- Night Float: 0 weeks
- NICU: 5 weeks
- Buddy: 4 weeks
- Epilepsy: 4 weeks
- CHP-OP: 4 weeks
- Psychiatry: 4 weeks
- Elective & Outpatient Clinic: 18 weeks
Our program now follows a 4+1 model with night float included.
Resident Clinic
Residents will participate in their own outpatient clinic week every 5 weeks. Residents will travel between AGH, Forbes, and Jefferson hospitals to precept with various faculty. This is a general neurology clinic, and patients with a wide range of disorders are seen. Every attempt is made to ensure that a cohort of patients follows each resident throughout their time here, allowing continuity and establishing important physician-patient relationships. At this time, resident will not be pulled into another service or work any weekend days.
Clinical rotations
Stroke Service
The stroke team consists of one senior and one junior, with a variety of rotators. The census consists of patients primarily admitted to the stroke service as well as patients on whom the stroke team is consulted. Patients are primarily located
in the neuroscience intensive care unit (NICU), the stroke unit, or the clinical decision unit (CDU). The team rounds on all patients each day, starting generally between 9 and 10 a.m. Residents on the service alternate weekends rounding on the team.
Admissions to the service are completed by the consult resident, buddy, or night float resident. Residents on the stroke service are not pulled away to do stroke
alerts, admissions, or consults.
General Neurology Service
The general neurology service consists of one senior and one junior resident, in addition to rotators on the service. The census consists of patients primarily admitted to the general neurology service as well as patients on whom general neurology is consulted. The team rounds on all patients each day, starting generally around 10 a.m. Patients present to this service with a wide variety of
pathologies, ranging from bread-and-butter to zebra. Opportunities in procedural
experience with lumbar punctures are plentiful.
Residents on the service alternate weekends rounding on the team. Admissions to the service are completed by the consult resident, buddy, or night float resident. Residents on the general neurology service are not pulled away to do admissions or consults.
Consult Service
The consult rotation is a unique opportunity for the participating resident to be involved in “first contact” history taking, examinations, and on-the-spot, sometimes acute, decision making. During this rotation, the residents are
responsible for taking all stroke alerts, admissions, and consults occurring
during the daylight shift. The patient is seen by the resident, properly staffed, and make decisions, including IV tPA and mechanical thrombectomy. For each case, the consult resident is expected to generate a sensible and comprehensive differential diagnosis, in addition to suggesting appropriate work-up and treatment. After this is done, the floater places the patient on an inpatient service, whether stroke or general neurology, or signs off as appropriate.
Buddy
The buddy rotation is functionally the same as the consult rotation, with the difference being that the buddy works in the evening, assisting the night float resident with all responsibilities. They have one weekday off per week.
Epilepsy
Each resident spends 2-4 weeks per year on a dedicated epilepsy rotation. This is an excellent opportunity to learn complex seizure and epilepsy diagnosis and
management. While on this rotation, the resident will admit all patients to the
Epilepsy Monitoring Unit for phase 1 and phase 2 evaluations and will additionally round on admitted patients with intractable epilepsy and status epilepticus. During the first year, the groundwork for reading and interpreting EEGs is laid through multiple daily reading sessions with an epileptologist, in addition the weekly EEG conference. These daily sessions continue into the second and third neurology years, refining the resident's skill in EEG. Finally, the resident participates in weekly epilepsy conferences by presenting difficult epilepsy cases to a group of physicians and experts from neurology, neurosurgery, radiology, and neuropsychology. Presentations include planning for patients that require intracranial monitoring, neuromodulatory devices, laser ablation, or resective surgery.
Night Float
Our program will no longer have a 24-hour call service but will have a dedicated Night Float resident throughout the night. This rotation will not exceed 2 weeks at a time.
Department Highlights
Comprehensive Stroke Center
The AGH Stroke Center is a nationally recognized leader in providing comprehensive and cutting-edge care for stroke patients. Our commitment to excellence is reflected in our designation as an Advanced Comprehensive Stroke Center by the Joint Commission, a distinction held by only a select few medical centers nationwide.
- Expert Care: Our multidisciplinary team of board-certified stroke specialists,
interventional neuroradiologists, neurosurgeons, and neurocritical care
specialists provides comprehensive and coordinated care for stroke
patients. - Advanced Technology: We are equipped with state-of-the-art technology, including:
- 3 MRI Scanners: With diffusion and perfusion weighted imaging capabilities for precise diagnosis and treatment planning.
- 4 CT Scanners: Equipped with CT angiography and perfusion imaging for rapid assessment and intervention.
- Digital Subtraction Cerebral Angiography: For advanced imaging and
treatment of complex stroke cases. - Transcranial Doppler and Carotid Ultrasound: For comprehensive evaluation and monitoring of stroke patients.
- Dedicated Stroke Units: We offer specialized care in our:
- 23-bed Neuro Intensive Care Unit: For critical care management of stroke patients.
- 36-bed Neuroscience Unit: For post-acute stroke care and rehabilitation.
- 42-bed Telemetry Monitored Unit: For close monitoring and management of stroke patients.
- Rapid Response System: Our LifeFlight aeromedical transportation system provides rapid transfer of stroke patients to AGH for timely and effective treatment.
- Comprehensive Training Program: Our neurology residents receive extensive training in all aspects of stroke care, including:
- Acute Stroke Management: Residents lead the acute stroke alerts, manage stroke patients in the emergency department, and make critical decisions regarding tPA administration, advanced imaging, and emergent endovascular procedures.
- Neurocritical Care: Residents provide primary care for stroke patients in the neurocritical care setting.
- Collaborative Care: Residents work closely with our multidisciplinary team, gaining valuable experience in managing complex stroke cases.
- Research and Innovation: We are actively involved in clinical trials and registries, including IRIS, CLEAR III, Clot Lysis, POINT, and GLORIA-AF, advancing our understanding and treatment of stroke.
Comprehensive Epilepsy Center
The AGH Epilepsy Program provides a comprehensive and innovative approach to the diagnosis, treatment, and management of epilepsy. Our team of experienced
epileptologists, neurosurgeons, neuropsychologists, and dedicated staff work
collaboratively to offer patients the most advanced and personalized care.
- Expert Care: Our team of four attending epileptologists provides specialized expertise in all aspects of epilepsy, from diagnosis to treatment.
- Cutting-Edge Surgery: We are a leader in epilepsy surgery, offering a full range of procedures including:
- Stereoelectroencephalography (SEEG): A minimally invasive
technique for precise localization of seizure foci. - Resections: Surgical removal of the seizure focus.
- Laser Interstitial Thermal Therapy (LITT): A minimally invasive
laser ablation technique for seizure control. - Device Placement: Implantation of responsive neurostimulation (RNS) and vagus nerve stimulation (VNS) devices for refractory epilepsy.
- Stereoelectroencephalography (SEEG): A minimally invasive
- Robust Training Program: Our neurology residents receive extensive training in epilepsy management through:
- Outpatient Epilepsy Clinic: Direct patient care and experience in managing epilepsy.
- ICU EEG Rounds: Experience in managing patients with status epilepticus and other critical neurological conditions.
- Epilepsy Monitoring Unit (EMU): Hands-on experience in the diagnosis and treatment of epilepsy.
- Weekly Epilepsy Surgery Conference: Participation in discussions and learning about the latest advancements in epilepsy surgery.
- Dedicated Epilepsy Monitoring Unit: Our EMU features 4 dedicated beds staffed by epileptologists, residents, technologists, and nurses. We are expanding this unit to meet the growing needs of our patients.
- Strong Inpatient Collaboration: Our inpatient neurology service works closely with the epilepsy service, ensuring seamless care for patients with seizures and status epilepticus.
- Advanced EEG Technology: Our EEG laboratory is equipped with 86 portable video EEG machines and 4 dedicated technologists, providing comprehensive and accurate EEG monitoring.
Neurodiagnostic Laboratory
AGH boasts a robust neurodiagnostic program, offering a comprehensive range of services and providing residents with unparalleled exposure to diverse neurological conditions.
EMG Expertise:
- Two dedicated neuromuscular specialists conduct approximately 1200 EMG studies annually, covering a wide spectrum of neuromuscular pathologies.
- Neurology residents actively participate in these studies, gaining hands-on experience alongside fellows, attending physicians, and EMG technicians.
- AGH's unique autonomic laboratory, one of few in the region, specializes in diagnosing small fiber neuropathies and other neuromuscular disorders.
EEG Excellence:
- The neurodiagnostic lab performs approximately 2300 EEGs annually, including both outpatient and inpatient services.
- The lab also conducts approximately 250 Continuous video EEGs per year, providing valuable insights into neurological activity.
- Six portable Natus/Xltek EEG machines, operated by four dedicated technicians, facilitate routine and long-term EEG monitoring across the hospital's nursing and critical care units.
- This comprehensive EEG program exposes residents to a vast array of EEG findings, spanning the ictal-interictal continuum.
Intraoperative Monitoring (IOM):
- AGH offers a comprehensive intraoperative monitoring service, staffed by two neurologists and nine dedicated IOM technicians.
- Residents interested in clinical neurophysiology are welcome to participate in elective rotations within the IOM program, gaining valuable experience in this specialized field.
This comprehensive neurodiagnostic program at AGH provides residents with an
exceptional learning environment, fostering their expertise in a wide range of
neurodiagnostic procedures and exposing them to the full spectrum of neurological conditions.
MS Clinic and Infusion Center
At AGH, we understand the unique challenges of living with multiple sclerosis
(MS). Our dedicated team of specialists, led by internationally renowned experts, is committed to providing comprehensive, compassionate care tailored to your individual needs.
Our Expertise:
- We have faculty with a leading authority on CNS inflammatory diseases, brings decades of experience and extensive research to our clinic.
- Our team is actively involved in ongoing clinical trials, contributing to the advancement of MS research and ensuring our patients have access to the latest therapies.
Personalized Care:
- Specialized MS Nurse: Our dedicated nurse provides ongoing support and education, ensuring you understand your diagnosis and treatment options.
- Multidisciplinary Approach: We collaborate with the National MS Society local chapter to offer a range of resources and support services.
- Comprehensive Diagnostic Evaluations: We utilize the latest diagnostic tools to accurately assess your condition and develop a personalized treatment plan.
- Training the Next Generation: Our neurology residents gain valuable experience in the diagnosis and management of MS, ensuring continuity of care for future generations.
- Convenient Infusion Center: Our outpatient infusion center provides a comfortable and safe environment for the administration of intravenous steroids and disease-modifying therapies.
ALS Certified Center of Excellence
Allegheny General Hospital stands as the only ALS Association-certified Center of Excellence for ALS in Western Pennsylvania, providing a vital resource for patients and families facing this challenging disease.
The ALS Clinic at AGH brings together a dedicated team of multidisciplinary professionals, including neurologists, physiatrists, social workers, speech
therapists, and pulmonary care specialists. This collaborative approach ensures
comprehensive care, diagnosis, and therapy for ALS patients, all under one roof.
The clinic's commitment to patient-centered care is evident in its track record of
supporting hundreds of patients and their families throughout the diagnosis and
treatment journey. By offering a comprehensive and coordinated approach, AGH's
ALS Center of Excellence provides a beacon of hope and support for those
affected by this debilitating disease.
Headache Center
AHN Headache Center is a fast-growing academic headache center in our community. The center was founded in 2017, has several branches and specializes in the treatment of patients with all types of headache pain. The clinical team consists of the Director, four additional neurologist, six APPs, full-times nurses, and numerous administrative and clerical support staff.
In addition to treating patients, AHN Headache Center is a teaching facility that gives residents the highest quality of preparation to make impactful contributions to patient care and advance the level of knowledge of headache medicine.
We are focusing on the multidisciplinary approach to collaborate with primary care providers, psychiatry, pain psychology, pain medicine and metabolic center.
We are in the process of establishing the Headache Fellowship program to prepare Fellows for a career in clinical headache practice or academic headache medicine and/or research.
Movement Disorder Clinic
The AGH Movement Disorder Clinic is dedicated to providing exceptional care for individuals living with Parkinson's disease, dystonia, tremor, and Huntington's disease amongst other movement disorders.
At AHN's Cahouet Center for Comprehensive Parkinson's Care, our team of highly skilled professionals, including Fellowship trained Neurologists assisted by physical therapists, occupational therapists, speech therapists, and psychologists work collaboratively to address the unique challenges associated with these complex conditions.
Neurologists work collaboratively with Neurosurgeons to provide the option of deep brain stimulators for qualifying patients.
Residents receive hands on experience in Botulinum toxin injections for patients with dystonia.
At the Movement Disorder Clinic, Neurologists actively participate in clinical trials and collaborate with leading researchers to develop innovative therapies to improve patient outcomes.

