AHN Neurosurgery Residency

Medical Students
If you're a medical student interested in our Neurosurgery Medical Student Program, please click here for more information.
AHN Neurosurgery Residency Program description
Welcome to the AHN Neurosurgery Residency website!
As a resident at AHN, you will be exposed to a wide variety of learning opportunities during your residency including clinical and didactic instruction as well as surgical exposure and training. A core group of faculty, fellowship trained
in specialty areas of neurosurgery who are genuinely interested and engaged in
teaching, will instruct and guide you as you develop and strengthen your clinical acumen in a collegial fashion while building and enhancing your surgical techniques. By the end of your residency, you will have established a strong and solid foundation of neurosurgery through which you will be readily prepared to practice neurosurgery - competently and independently.
An organized faculty and resident driven curriculum highlights information essential in caring for neurosurgical patients as well as for passing the ABNS Primary Examination. The AHN Written Board Review Series and the Myers Board Preparatory Sessions provide a structured approach to studying high yield material. The curriculum, inspired by the ACGME core competencies, focuses also on practical physician development topics including professionalism, ethics, diversity, and socioeconomics. The AHN Neurosurgical Resident Research Council will teach you the key concepts and principles of research though one-on-one meetings with scientists and core faculty. Lecture series and workshops and will help you develop your personal research interests early in your training and provide you with the tools and foundation to be productive and enable you to meet your personal research goals. As your fundamental knowledge of neurosurgery deepens, your surgical skills will be augmented via a curriculum focused cadaveric dissection BIOSKILLS laboratory sessions as well as
opportunities for independent cadaveric dissection in our Center for the Surgical Arts. A myriad of AHN sponsored courses are also available to supplant your education as well as build your personal network of connections with surgical colleagues nationally and internationally.
You will be introduced to the field of neurosurgery as a PGY 1 through a “buddy system” where you will be exposed to the duties of a neurosurgical resident under the direct supervision of a senior resident for all aspects of patient care including bedside procedures and call. During this first year, you will also be introduced to other surgical subspecialties to teach you basic surgical techniques, critical care, and patient management skills to develop your clinical acumen. By PGY 2, you will be able to function independently in taking care of neurosurgical floor and ICU patients under the supervision of senior residents and faculty. During PGY 3, you will be exposed to various neurosurgical specialties as well as electives pertinent to neurosurgery. PGY 4 and 5 are surgically concentrated. During PGY 5, you will rotate through Forbes Regional Hospital, part of the AHN system, which will prepare you for your ensuing role as Chief Resident as a sixth year resident. During PGY 7, you may elect to complete an enfolded CAST fellowship, an elective fellowship, a focused research year, or a “transition to practice” year.
Policies and procedures to which residents must adhere to include those of the AHN Department of Neurosurgery and those of the AHN Graduate Medical Education (GME) Office.
For more information, please explore the information on this site. We sincerely thank you for your interest in the AHN Neurosurgery Residency program.
AHN Neurosurgery Residency Program year and rotations
See below for breakdown of individual rotations as they occur by each post-graduate year. A brief description of the rotations follow PGY listings.
PGY 1
- Plastic Surgery - 1 month
- Trauma ICU - 1 month
- Emergency Department - 1 month
- Neuropathology & Neuroradiology/SRS - 2 months
- Introduction to Neuro-Critical Care - 1 month
- Neurosurgery - 6 months
PGY 2
- Neurosurgery/Neuro-Critical Care - 12 months
PGY 3
- Pediatric Neurosurgery - 4 months
- Endovascular Neurosurgery – 4 months
- Neurosurgery - 4 months
PGY 4
- Neurosurgery - 8 months
- Functional Neurosurgery - 4 months
PGY 5
- Forbes Neurosurgery – 6 months
- Neurosurgery – 6 months
PGY 6
- Chief Year
PGY 7 (one of the following)
- Elective Year
- Research
- Enfolded CAST Fellowship
- Elective Fellowship
- Transition to Practice
Emergency Medicine (EM)
The goal of this rotation is to become familiar with the initial assessment and management of patients in the acute setting. This rotation is helpful in not only basic clinical knowledge but also will aid in preparing for the USMLE - Step 3 Examination.
Endovascular Neurosurgery
This rotation is a 4 month, protected rotation, on the neuro-endovascular service, during which the resident will perform all neuro-endovascular procedures, learn to manage variety of vascular pathologies, and take stroke call.
Forbes Neurosurgery
For 6 months during PGY 5, resident will act as a junior attending at Forbes Regional Hospital, a level 2 trauma center part of the AHN system. The operative experience of the rotation focuses on complex spine and adult deformity as well as general neurosurgery.
Neuropathology
Goals and objectives of this rotation are that the resident understands the basic pathological features and pathological processes of common disorders of the nervous system. This training will help the trainee to pass the board exam and to offer better patient care by understanding neuropathology.
Stereotactic Radiosurgery
Goals and objectives are for the resident to acquire requisite background information to understand the indications for and the various techniques used to perform radiosurgery, as well as directly aiding in planning and execution of stereotactic radiosurgery.
Neuroradiology
Goals and objectives for this rotation are that the resident will become thoroughly familiar with all aspects of neuroradiology, including myelography/CT, angiography/CT, MRI, and neurointerventional procedures.
Pediatric Neurosurgery
During PGY 3, the neurosurgery resident will rotate 4 months at UPMC Children’s Hospital; attend all required pediatric conferences; take call as scheduled by the pediatric chief resident; and participate in outpatient clinics and inpatient consultations.
Goals and objectives of the rotation are to provide an educational pediatric neurosurgery experience in patient care activities. The resident will gain knowledge in the anatomy, physiology, pathophysiology, and presentation of diseases in children that a neurosurgeon may be called upon to diagnose and treat.
Plastic Surgery (PS)
The primary function of this rotation is to learn management of complex wounds and proper surgical techniques. The rotation consists of heavy operative days as well as management of plastic surgery consult and floor patients.
Trauma ICU (TICU)
The goals and objectives of the Trauma ICU rotation are to learn comprehensive management of trauma patients, including coordinating care of patients with head and neck, chest, abdomen, and extremity injuries and treatment plans for severe soft tissue and pulmonary infections, respiratory failure, hemodynamic instability, renal failure and major bleeding.
Introduction to Neuro-Critical Care
During the PGY 1 year, the neurosurgical residents will be scheduled for an initial “Intro to Neuro-Critical Care” rotation in the Neuro ICU. This rotation will be an initial exposure to the basic foundations necessary for management of the critically ill patients in the NICU setting including the basic principles of critical care medicine, neurology, neuroanatomy, neurosurgery, and neuro-interventional radiology with direct supervision available at all times.
AHN Neurosurgery Residency Program block rotation schedule
Attached is a chart detailing the AHN Neurosurgery Residency Program block rotation schedule.
AHN Neurosurgical Residency Program academic monthly calendar
Academic Week
Tuesday Mornings - 6:30 AM - 8:00 AM
Wednesday Mornings - 6:45 AM - 12:00 PM
Tuesday Mornings
1st Tuesday
- NSG Resident Research Council (6:30 AM - 8:30 AM)
2nd Tuesday
- Compliance / Well Being (6:30 AM - 8:30 AM)
3rd Tuesday
- Written Board Review Series (7:00 AM - 8:00 AM)
4th Tuesday
- Written Board Review Series (7:00 AM - 8:00 AM)
Wednesday Mornings
Every Wednesday
- NSG Internal Conference (6:45 AM - 7:20 AM)
- Neuroscience Institute Grand Rounds (7:30 AM - 8:30 AM)
- Myers Board Prep (8:30 AM - 9:30 AM)
1st Wednesday
- Neurosurgical Lecture Series (9:30 AM - 10:30 AM)
- Neurosurgical In-services (10:30 AM - 12:00 PM)
2nd Wednesday
- BIOSKILLS Cranial (9:30 AM - 12:00 PM)
3rd Wednesday
- Neurosurgical Lecture Series (9:30 AM - 11:30 AM)
4th Wednesday
- Neurosurgical Lecture Series
5th Wednesday
- Neurosurgical Lecture Series (9:30 AM - 10:30 AM)
- Neurosurgical In-services (10:30 AM - 12:00 PM)
Example Neuroscience Conference Schedule
Attached is an example of the Neuroscience Conference Schedule.
AHN Neurosurgical Residency Program curriculum highlights
- BIOSKILLS Laboratory Sessions
- Myers Board Prep
- Written Board Review Mini Series
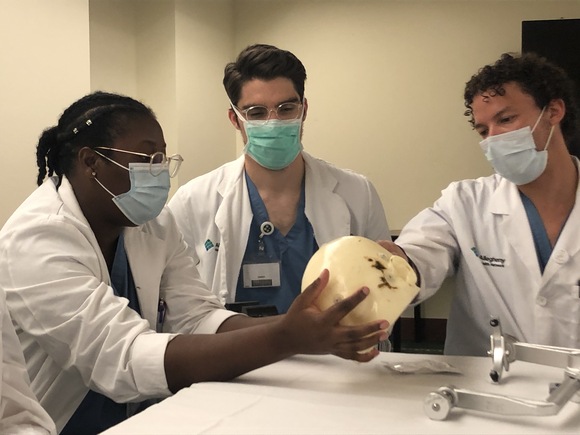

Laboratory Sessions
At AHN, we have access to a premier cadaveric facility, Center for the Surgical Arts, available for personal education as well as a part of the structured curriculum. Residents will have protected laboratory time for a focused study in one of the many cranial or spinal surgical approaches. These sessions are proceeded by a lecture prepared by a resident and are supervised by faculty members. Each lecture includes the following:
- Brief case presentation with imaging
- Specific indications for the procedure
- Anatomy associated with the approach
- Surgical approach
- Alternative approaches and treatments
- Common pitfalls and pearls
- Outcomes associated with the approach (1-2 articles briefly presented/reviewed)
Following the presentation, the group then proceeds to the laboratory where they perform the approach with the assistance of faculty members. Various operative equipment such as surgical robots, CT navigation, intracranial endoscopes, an fluoroscopy are available during these sessions to simulate the actual operative experience. Residents are often exposed to innovative technology on trial during these sessions as well.

July - N/A
August - 8/9/2023 Pterional, FTO, FTOZ/Interfacial/Subfacial
September - N/A
October - 10/11/2023 Fiber Dissection
November - N/A
December - 12/13/2023 Middle Fossa/Approaches to Cavernous Sinus
January - N/A
February - 2/14/2024 Retrosig/Far Lateral
March - N/A
April - 4/10/2024 Suboccipital/Telovelar/Pineal
May - N/A
June - 6/12/2024 EEA Anatomy

July - Posterior Cervical Laminectomy / Cervical Decompression and Fusion (including T1 and T2 Pedicle Screws)
August - Anterior Cervical Discectomy and Fusion / Cervical Artificial Disc / Cervical Corpectomy
September - Lumbar Microdiscectomy and Laminectomy
October - Open Lumbar Pedicle Screw Placement and Instrumentation (PLIF, TLIF) including S2 Screws
November - Peripheral Nerve (Brachial Plexus, Carpal Tunnel, Ulnar Nerve Decompression)
December - Sacroiliac Joint Fusion
January - Robotic/ Navigation Assisted Percutaneous Thoracolumbar Instrumentation; Transpedicular Discectomy
February - Deformity Correction (Smith-Peterson Osteotomy, Pedicle Subtraction Osteotomy, Vertebral Column Resection)
March - Anterior/ Oblique/ Lateral Thoracolumbar Fusion
April - Minimally Invasive/ Tubular Approach to Cervical and Lumbar Pathologies (including Far Lateral Approach)
May - Posterior C1 and C2 Fixation (C1 Lateral Mass, C2 Laminar, C2 pars, Transarticular); Occipito-Cervical Fixation
Myers Board Prep
Myers Board Prep is a resident organized and driven board preparatory course occurring on a weekly basis throughout the entire academic year geared to residents taking the Written Board Examination. The residents are assigned topics at the beginning of the year. The curriculum is organized at the beginning of each academic year and is integrated with the BIOSKILLS laboratory sessions schedule to facilitate comprehensive understanding of the basic neurosciences applied to related surgical approaches.
Testimonial

“At the start of residency, preparing for and passing the Neurosurgery Written Boards can be a daunting if not overwhelming task. We have revamped our entire approach to written boards over the last few years to try and minimize the stress of preparing for boards, and to maximize its benefit to us as clinicians. As a group, the residents who still need to pass written boards focus on a board exam topic that is of clinical utility every week.
As we move through the year, the idea is not to only improve our knowledge base, but to deescalate the stress surrounding the written boards. So far this has been extremely successful in terms of our education, stress level, and the board scores!”
-Daniel Myers, MD
PGY 6
About Graduate Medical Education
The Neurosurgery Residency program is part of the Graduate Medical Education (GME) opportunities offered by the AHN Medical Education Consortium. Learn more about Graduate Medical Education.
Contact us

Program Coordinator
Mailing address:
AHN Neuroscience Institute at AGH
Department of Neurological Surgery
320 East North Ave
Hemlock Building, 5th Floor
Pittsburgh, PA 15212
Phone: (412) 359-3047
By accessing this video, I understand that I am leaving the AHN website and I will be re-directed to an external website operated by a third party platform provider. I acknowledge that the platform provider may collect personal information about me, and about the video that I view, on their platform and may use and disclose this information in accordance with its privacy policy. I agree that Allegheny Health Network is not responsible for the data collection and use practices of this third party.

