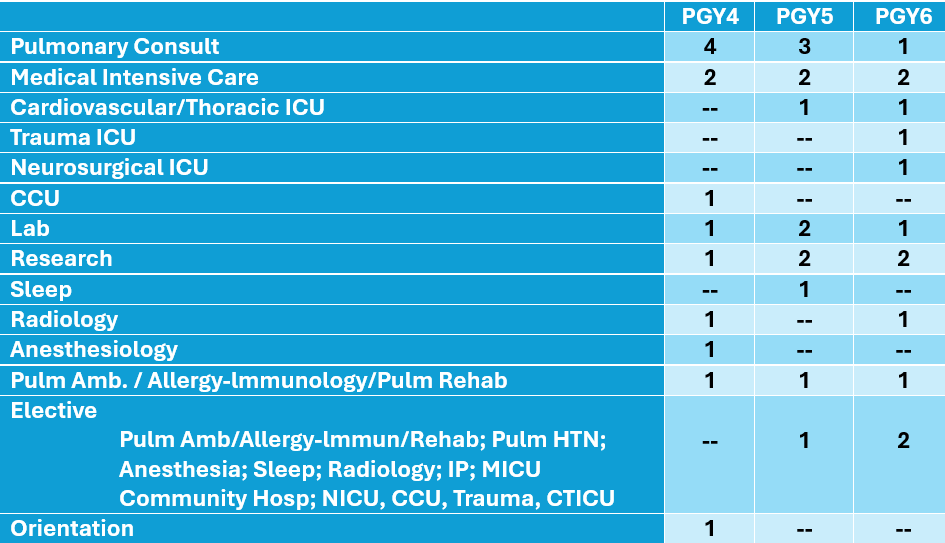
Pulmonary and Critical Care Medicine Fellowship Curriculum
Schedule
Orientation
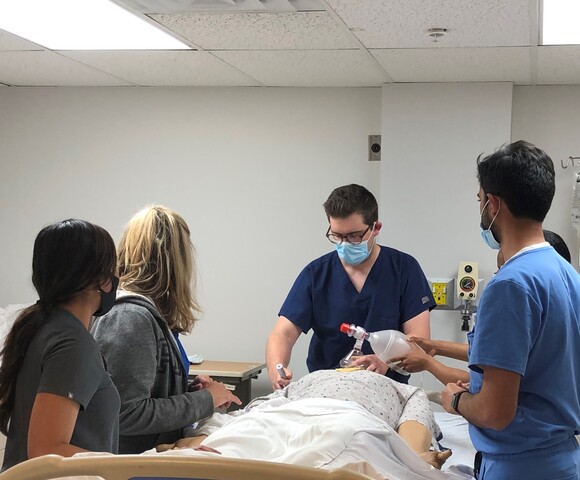
Fellowship commences with a month of orientation, during which the first year fellow will become competent in basic ICU procedures, including central lines, arterial lines, and chest tubes gaining an understanding of the indications and complications of these procedures. The fellow will work alongside an attending and senior fellow during this month in both the medical intensive care unit and pulmonary consult
service.
Each first year fellow will also participate in:
- STAR Center Skills Simulation Lab
- Cadaver Lab Experience- one-day course
- Central and arterial line
- Direct Laryngoscopy
- Glidescope Intubation
- Bronchoscopic Intubation
- Bronchoscopy
- Pigtail Chest tube placement
- Surgical Chest tube placement
- IO Placement
- Blakemore insertion
- Emergency cricothyrotomy
- Ventilator Course
- Ultrasound Course – Standardized patient course will review
- Vascular - access and anatomy
- Thoracic – pleural, lung and pneumothorax
- Abdominal - ascites, bowel and bladder, renal; and
- Cardiac - image acquisition and interpretation.
- Module ultrasound training also available
Pulmonary Consults
The pulmonary consult rotation is a dedicated teaching service with 2 fellows per month, rotating residents, medical students, and teaching attending. During this rotation the fellows gain competency in clinical knowledge, management skills, and procedural skills in all aspects of pulmonary medicine. Fellows are responsible for coordinating treatment plans, procedures and for the subsequent follow up of these patients. The most senior fellow on rotation will serve as a “junior attending” and lead the team of residents and medical students. 9 months of consults will be required over the 36 months of training. A cap has been created to ensure the educational experience is of the utmost importance.
Lab rotation

The lab rotation is dedicated to learning and gaining competency in all aspects of bronchoscopy, including diagnostic, therapeutic, endobronchial ultrasonography, transbronchial biopsy, cryobiopsy, endobronchial blocker placement, endobronchial valve placement, supraclavicular lymph node biopsy, and navigational bronchoscopy under the direction of our interventional pulmonary team. The fellow will perform bedside tracheostomies and tunneled pleural catheter placement.
ICU Rotations

Medical ICU
Our fellows generally have 6-months of MICU training, which
encompass all aspects of critical care, including cardiac arrest, ARDS, PE, shock, respiratory failure, upper and lower GI bleeds, liver failure, hematological/oncological emergencies, toxic and metabolic disorders, and renal disorders. During these months, fellows will learn conventional and unconventional modes of mechanical ventilation. As the fellow progresses their role will become that of a Junior Attending leading MICU team rounds. This graduated responsibility provides the fellow more autonomous growth and confidence in handling an ICU upon graduation.
Trauma
AGH is a Level 1 Trauma Center. During the Trauma ICU rotation fellows will learn primary and secondary surveys, respond to trauma codes with the trauma team, participate in and lead trauma rounds, and perform critical care procedures.
Cardiovascular/Thoracic ICU Rotation
The fellow will gain experience with VA and VV ECMO, pulmonary artery catheters, mechanical devices, post-operative care of cardiothoracic patients, and the management of those patients admitted to the intensive care unit following coronary artery bypass graft surgery, valvular heart surgery, thoracic surgery, and solid organ transplant.
Neurosurgical ICU
AGH is a comprehensive stroke center and has a robust neurosurgical service. The fellow will rotate daily with the neurosurgical team and board-certified neurointensivists.
Sleep
Pulmonary Critical Care Fellows rotate through the Sleep Disorders Center at AGH during their second year. This is a multidisciplinary program that evaluates, diagnoses and treats all sleep disorders. The fellow will interact with many medical disciplines including Sleep Dentistry, and Sleep Psychiatry.
Radiology
Working with AGH Thoracic Imaging Radiologists, fellows will obtain instruction and knowledge of the indications, interpretation. and differential diagnosis of the key chest imaging.
Anesthesiology
This rotation allows the fellow to gain airway skills in the non-emergent
setting. Skills include bag mask ventilation, LMA insertion, and endotracheal intubation with direct laryngoscopy and glidescope.
Research

Fellows are encouraged to select research projects based on their interests. The Medicine Institute provides research coordinators statisticians and medical writers. Fellows are required to present research at national meetings and participate in research projects throughout their fellowship.
Ambulatory care
Faculty Offices
Fellows are assigned to a “clinic attending” for 36 months of their training. Through these half or whole day sessions, the fellow will develop graduated responsibility and autonomy as competency is acquired. The faculty offices allow the fellow to gain knowledge in the diagnosis, management and longitudinal follow up of patients with various types of lung diseases.
Breathing Disorders Center
Fellows will have the opportunity during their ambulatory care experience to rotate through the Breathing Disorders Center, a full service pulmonary practice with a strong focus on the management of chronic respiratory disorders through evidence based protocols.
Tuberculosis Clinic
Fellows are also provided experience at the Allegheny County Health Department Tuberculosis Clinic, under the direction of Dr. Eric Bihler. This is a rather unique opportunity to care for patients who have latent and active TB.
Interventional Pulmonary Clinic
While fellows are on their lab rotation, they will attend IP clinic. Procedures performed include thoracentesis, lymph node aspiration, and tunneled pleural catheter management. In IP clinic, the fellow will also evaluate and manage nodules, evaluate patients for endobronchial valves and stent placement.
ILD Clinic
Fellows can rotate at the multi-disciplinary ILD clinic working alongside rheumatology evaluating patients with various autoimmune conditions with pulmonary involvement.
Post Intensive Care Syndrome Clinic
Fellows have the opportunity to provide longitudinal care for ICU patients in the PICS Clinic working alongside pharmacy, nursing & social workers.
Asthma Clinic
Fellows will get further exposure to difficult-to-treat asthma in this specialized clinic.
Conferences

Our comprehensive conference schedule enhances to the fellows clinical training. Conference schedule includes:
- X-ray Conference
- Thoracic Oncology Case Conf. - Multidisciplinary
- Journal Club – Pulmonary and Critical Care
- Take 5 – reviewing the latest literature
- Case Conferences -- Pulmonary and Critical Care
- Core curriculum didactic lectures
- Board Review
- M&M case review and RCA conference
- Physiology review
- Interactive Clinical Case Series
- Interstitial Lung Disease Case Review – Multidisciplinary
- Research/Quality Improvement Conference
- Ultrasound bedside rounds
- Ventilator bedside rounds
- The Division has three multidisciplinary conferences that include faculty and house staff from the Department of Cardiothoracic Surgery, Pathology, Radiology, Oncology, Nephrology, Infectious Disease and Rheumatology. Fellows present current cases to the multidisciplinary faculty to optimize diagnostic and treatment plans as well as patient outcomes.
Annual Courses
- Cadaver Procedure Lab
- Simulation Procedure/Codes
- Ventilator Management
- Ultrasound Procedure
- Difficulty Airway